11 Wisdom
Becoming a wise physician
Caring for infants and children with complex congenital heart disease is one of the most challenging and complicated areas of medical practice. When I completed my pediatric fellowship, I briefly considered focusing my clinical practice and teaching in this area. I soon realized that my ambitions and growing responsibilities in the realm of medical education, which included recruitment, curriculum development, and meetings, would prevent me from participating in the full-time staffing of cardiac cases in the operating rooms. While I had to make an early career decision to focus on my nonclinical academic interests, I hoped to continue my connection to this fascinating patient population by caring for infants and children with congenital heart disease in the cardiac catheterization laboratory (CCL) for diagnostic and interventional procedures and in the operating rooms for noncardiac surgery.
When I committed to caring for this special group of patients, I felt an obligation to continue acquiring the knowledge, experience, and judgment needed to maintain a high level of competency in this area of practice. There are few areas of medicine that require such commitment to continuing education and patient-centered medical practice as caring for infants and children with congenital heart disease. The permutations for clinical presentation within each diagnosed lesion are infinite and quite varied in severity. In addition, complications in care can arise from the comorbid conditions that coexist in these children, such as prematurity with neurological delay, respiratory failure, and genetic disorders. It was customary for each child to be evaluated by a multidisciplinary team of subspecialists prior to any procedure, a practice that rightly reaffirmed the uniqueness of each child. The families were also unique and inspiring in their commitment to prolonging the life of their child, empowering the physicians and nurses that cared for their child even further.
If I was going to care for children in the CCL, I needed to maintain familiarity with the members of the multidisciplinary team, their respective areas of expertise, and the range of cardiac procedures performed to gain the respect of my colleagues. Self-awareness, trust of colleagues, adept communication skills, and clinical competency would be critical to providing effective care, especially in the event of acute medical crises. A major component of advancing my knowledge and competency was devoting myself to learning about the various cardiac lesions associated with congenital heart disease and its anesthetic management, which involved identifying the best peer-reviewed articles and other reference materials. And finally, I was committed to doing complex cases, attending cardiac conferences, and consulting more experienced colleagues.
After a few years, I believed I had achieved satisfactory competency in this area of practice. I had also gained the confidence and self-awareness to acknowledge when a more experienced colleague would be better suited for a few of the most complex cases in the CCL or in the operating room. When I was scheduled with one of our pediatric fellows to care for an infant with hypoplastic left heart syndrome (HLHS) who had recently completed the first stage of his palliative repair with the placement of a Blalock-Taussig Shunt (BTS), I was confident in my ability to care for this infant for a straightforward general surgery procedure. It is beyond the scope of this story to explain the complicated underlying pathophysiology of HLHS, describe a BTS, or discuss the implications of the resultant cardiopulmonary physiology for surgical and anesthetic management. Suffice it to say, all members of the team proceeded with caution and continuous communication, as any procedure would be considered high risk for an infant with this underlying condition. During our “time out” prior to beginning the surgery, we all discussed our specific concerns to further raise the team’s awareness of potential complications.
Approximately 30 minutes into the procedure, the infant experienced a sudden decrease in oxygen saturations with concomitant hemodynamic instability. The infant’s status did not improve despite multiple resuscitative interventions, including cessation of the surgical procedure. The cardiac surgery team that had just placed the BTS was fortunately in an adjacent operating room and was consulted emergently. They felt the instability was most likely secondary to either hypovolemia or our ventilation strategy. Following our initial resuscitative efforts, I felt we had already addressed both these issues. I wondered if the surgical team should be placing a possible problem with the BTS higher on the differential diagnosis for the acute onset of refractory hypoxia and hemodynamic instability. I suggested we call the pediatric cardiologists to take the child to the CCL emergently to investigate the integrity of the BTS. After some debate and consulting a pediatric cardiologist, the cardiac and general surgery teams agreed to do an emergent cardiac catheterization. The communication, decision-making, and collaboration resulted in an impressive and seamless transfer of this unstable infant to the CCL. The cardiac catheterization procedure started within a few minutes.
I was relieved when the pediatric cardiologist immediately focused on the BTS and discovered it was occluded by a blood clot. They were able to remove the thrombus within minutes. The infant’s hemodynamic status and oxygenation immediately returned to normal. Following a period of careful observation in the CCL, the infant was transported to the critical care unit in stable condition. His surgical procedure was rescheduled.
In the aftermath of this event, a multidisciplinary case review occurred involving all team members. Each participant was given an opportunity to share their perspective in a safe environment. After considering all the information and ideas that were offered, the cardiac service implemented some new quality improvement strategies surrounding the care of infants with HLHS following the placement of a BTS. This included a change is the management of anticoagulation during the perioperative period for noncardiac surgery to preclude the development of a thrombus.
I learned early in my career that good decision-making results from acquiring the knowledge and experience to problem-solve using all available resources, bracketing any innate biases. I have tried to remain curious and open-minded in all facets of my professional and clinical practice, which I believe is essential for maintaining competency. This case demonstrated that multidisciplinary teams deliver optimal and lifesaving care when there is trust, open communication, and a willingness to embrace a variety of perspectives to problem-solve.
Key Concepts
- Acquiring knowledge and skill is a lifelong commitment for physicians.
- Humans retain cognitive biases that negatively impact our ability to learn, creatively problem-solve, and work in multidisciplinary practice.
- When you understand your competencies, biases, and limitations, you have become wise.
One definition of wisdom is the quality of having the knowledge, experience, and judgment necessary to make good decisions and provide thoughtful counsel. Early philosophers addressed the topic of wisdom in their writings. Socrates believed that genuine wisdom begins with acknowledging the limits of our knowledge with humility. He argued that when we think we know everything and are unwilling to admit our ignorance, we close ourselves off to learning and growth. Aristotle shared this idea, saying, “The more you know, the more you know what you do not know.” The common theme is that acquiring wisdom means knowing your limitations and being aware of your deficits in knowledge and experience. Developing wisdom takes time and patience as you acquire foundational knowledge in your profession, gain perspective through experience, and have opportunities to develop sound judgment in your medical practice. As in the above story, medical crises test the limits of your knowledge, skill, and judgment. It is at these times that your confidence and the strength of your convictions are challenged.
If you remain receptive to feedback from supervisors and patients, you have ongoing opportunities for self-assessment. Multi-source evaluations from colleagues serve as a particularly useful tool for self-reflection, given your peers’ familiarity with your practice and their informed perspective. Non-physicians provide unique insights regarding your ability to communicate with patients and colleagues in a professional manner. Self-awareness gives you the ability to provide balanced counsel to your patients when discussing complex medical issues and obtaining informed consent. I have described empathy as an essential attribute of physicians who wish to forge positive physician-patient relationships that build trust and enhance compliance with prescribed medical therapies. As we seek to understand other perspectives and remain open-minded to new ideas, we approach our own decision-making with greater objectivity and judicious analysis. Though accomplished in their respective fields, many of your most inspiring role models were probably very humble and self-aware individuals.
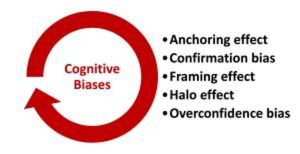
Common cognitive biases in medicine
With wisdom comes a greater awareness of the many cognitive biases that negatively impact your decision-making. It is important that you be able to step back and reconsider a conclusion prior to making high-stakes decisions, as this practice helps you avoid letting your past experiences or conventional wisdoms overly bias future decisions. I remember early in my career being influenced by my most recent experience or the initial counsel of a trusted mentor. I lacked the experience to fully understand the nuances surrounding complicated patient and family medical decisions. The anchoring effect is our tendency to be overly influenced by our first experience, bit of information, or data point. You can address this innate predisposition by considering alternative diagnoses or treatments for patients with a condition, referencing objective evidence-based guidelines and protocols. One of the most effective tools for countering anchoring bias is collaborating and consulting with colleagues in a multidisciplinary practice model. The Socratic method of learning and teaching combined with frequent multidisciplinary case conferences where there is collegial and constructive debate reinforces the value of objective and collaborative decision-making.
You will develop beliefs and attitudes that you instinctively want to confirm and sustain in your career. Confirmation bias is probably the most difficult bias to overcome as a professional. When specific practices reaffirm deeply held values, some find it difficult to accept alternative ways of addressing an issue or problem. We are all prone to rely on familiar methods of problem-solving, which can lead to cognitive rigidity and prevent you from considering another viewpoint when making decisions. Remaining flexible and open to different perspectives enables you to broaden your knowledge and clinical practice over time. Many multi-source assessments of physicians that focus on professionalism and communication skills ask a physician’s colleagues to comment on the physician’s willingness to listen to others, work collaboratively, and remain open to new ideas. These traits combat confirmation bias and are considered foundational professional attributes.
How information is presented can influence your decision-making. The framing effect is a cognitive bias that challenges your ability to remain objective when information is presented in a fashion that is recognizable and easily understood, especially if it is presented in a positive manner. It is convenient to accept initial data as being definitive, especially when it is consistent with a previous diagnosis that has followed a similar pattern. Though it is often expedient to act according to such patterns, you should remain open to alternative diagnoses when additional studies indicate it would be appropriate to reach a fully informed decision. It is also important for physicians to be mindful regarding how they present information to patients, especially when providing medical counsel and obtaining informed consent. An example of potential framing bias in medical practice surrounds how you present the risks and benefits of a planned surgical procedure. If a patient is informed that a procedure has a 90% success rate without complications, they are probably more likely to consent to the procedure compared to being told that the surgery has a 10% risk of complications with a detailed discussion. Though both descriptions of the risk-benefit are true, presenting only the positive potential without mention of the negative unintentionally minimizes the risk. For elective surgery, it is frequently the impact of postoperative recovery on a patient’s quality of life that needs to be properly framed and balanced with the overall benefit of the procedure.
Mentors, role models, or other individuals who make a positive first impression impact our assessment of their expertise, leading us to overestimate and exclusively rely on their opinion. The halo effect is a recognized cognitive bias that increases an individual’s influence on your decision-making. In the traditional hierarchy that exists in medical training and practice, seniority is often the basis for deserved respect and influence over the learning and practice of junior colleagues. While this hierarchy is an important component of teaching and mentorship, part of your professional identity formation is developing an ability to separate opinion from fact using the best available evidence. Influencers are common in society and are now used by companies to market a product. In medical practice, we fortunately have access to objective information and examples of best practices to fact-check a trusted colleague’s consultation.
Despite being a highly educated physician, you are susceptible to developing overconfidence bias. It is essential that you recognize this vulnerability and that you remain humble and cognizant of the limits of your knowledge and skill. Understand that you always have more to learn. Overconfidence bias is a challenge at any stage of your career. When you are acquiring the foundational knowledge and skills necessary to become a competent practitioner, there are times where due to lack of self-awareness, you overestimate your ability to perform a given task. Self-awareness remains a core attribute of physicians throughout their careers. Patient satisfaction and positive clinical outcomes ultimately provides confirmation of your adherence to evidence-based medical care and overall competency.
When there has been an unexpected adverse event or “near miss” where a bad outcome was narrowly avoided but there could have been errors in judgment, an important component of a comprehensive quality assessment and improvement program is to perform a multidisciplinary review of the event. This review process often starts by conducting private and confidential interviews with all individuals involved in the care of the patient. Any others who witnessed the event but did not provide care are also frequently interviewed. These reviews are inherently stressful, especially since caregivers are commonly still dealing with the emotional impact of the event. Reviewers are sensitive to these feelings and to inherent biases that exist. In my role leading some of these reviews, I sometimes began the review process by interviewing the least experienced observers and caregivers, starting with open-ended questions about their observations. I found their recollections tended to be the least biased in their roles as novice observers and non-stakeholders. On the other end of the spectrum, the most senior physicians and nurses who were directly involved in the care were often more guarded, sometimes responding to open-ended questions with phrases such as “I have done this procedure a thousand times” or “I have never had a bad outcome.” These types of responses are not necessarily indicative of a deliberate attempt to avoid accountability but are more likely illustrative of common cognitive biases that exist in medical practice. As physicians, we should strive to maintain objectivity as we support and participate in quality improvement initiatives. I have been the beneficiary of a colleague’s expertise and more objective observations when conducting reviews of my own clinical practice.
There are deliberate strategies you can utilize to prevent cognitive biases from impacting your judgment. Conducting periodic reviews of the most recent clinical and translational research and of updated clinical practice guidelines provides you validated best practices. Checklists and decision-making algorithms are becoming an important component of quality improvement initiatives. Colleagues also serve as another objective resource when you face difficult professional and clinical decisions. Your patients periodically provide you opportunities to revisit a decision when they question a diagnosis or treatment plan. Physicians should always be receptive to reconsider a conclusion when challenged, especially if there is a possibility of personal or institutional bias.
Suggested Reading
- Masic I. Medical decision making – an overview. Acta Inform Med (2022) 30(3):230-235. DOI: 10.5455/aim.2022.30.230-235
- Hammond M, Stehlik J, Drakos S, Kfoury A. Bias in medicine: lessons learned and mitigation strategies. JACC: Basic to Translational Science (2021) 6(1):78-85. DOI: 10.1016/j.jacbts.2020.07.012
- Webster C, Taylor S, Weller J. Cognitive biases in diagnosis and decision-making during anaesthesia and intensive care. BJA Educ (2021) 21(11):420-425. DOI: 10.1016/j.bjae.2021.07.004